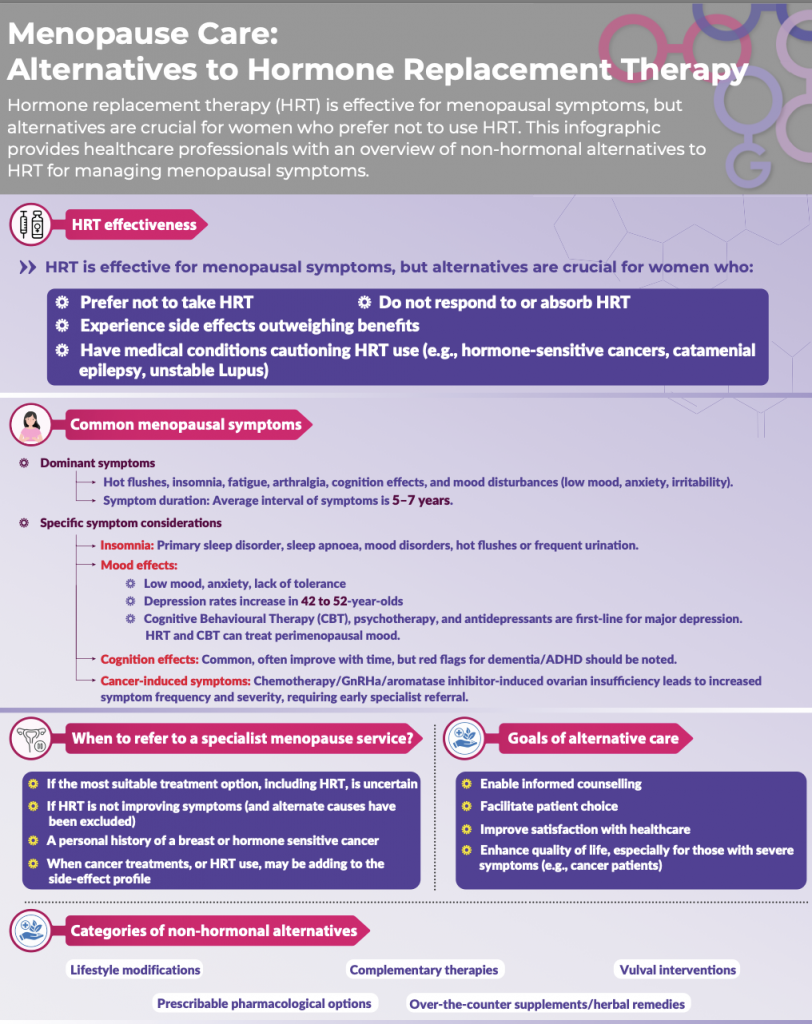
There are many ways of managing your menopause symptoms and support your wellbeing that do not involve adding hormones. Many women do not want to take hormones, or are unable to take hormones. They can be made to feel that there are no other options for them to help reduce their symptoms.
At Rowena Health we take a holistic, patient centred approach and this involves us listening to what is important to you, what you have experienced in the past and together we can talk through all of the options to help guide you to decide on the right treatment for you. There are many options which do not involve taking hormone replacement therapy.
Few complementary and alternative treatment options have proven evidence to show how effective they are, and although they do not stand up to scrutiny from a robust and evidence-based perspective, there are individual women who benefit from these treatments.
Bio-identical hormones should not be considered an ‘alternative’ to HRT. There is limited evidence about their effectiveness and safety.
Healthy lifestyle choices
See our lifestyle FAQ for helpful information about the lifestyle pillars. There might be some changes you can make to your lifestyle to help relieve your symptoms.
Stopping smoking, keeping alcohol intake low, wearing light cotton layers, avoiding caffeine and spicy foods, and using cooling aids such as gel packs or fans at night can all help reduce hot flushes. High-impact exercise can sometimes make flushes worse.
Regular moderate-intensity exercise is beneficial. Aim for at least 30 minutes 5 times a week, but to manage weight loss and maintain your weight, increasing this level to an hour a day (300 minutes a week or more) can be helpful. High-intensity activity, particularly in the evening or close to bedtime, can sometimes make it harder to sleep. Adding strength exercise 2-3 times a week. Practice balancing to help you avoid falls later in life and don’t forget those pelvic floor exercises.
Gentle activities such as yoga, Pilates, and Tai Chi can ease joint stiffness, lift mood, improve energy, and support mental focus.
There’s increasing evidence that gut health plays a role in joint pain and other menopause symptoms. Eating in a way that supports a healthy gut, reducing saturated fats and ultra-processed foods may also have positive effects on mood and cognition.
Managing other health factors like blood pressure, blood sugar, hearing, weight, mood, and social connection can help protect cognitive function. Although losing weight can be more difficult during menopause, even small reductions can improve joint pain and hot flushes. Interestingly, newer medications known as GLP-1 receptor agonists (used for weight management and diabetes) may also help reduce the frequency and intensity of flushes.
Cognitive behavioural therapy (CBT)
CBT can help to improve anxiety, depression, sleep, and vasomotor symptoms (hot flushes and night sweats). CBT can be arranged as individual 1-1 therapy, in a group session or by using an online course or a book to support you.
- Women’s health concern fact sheet CBT
- Book: Managing hot flushes and night sweats by Myra Hunter
- Sleep CBT for insomnia: have a look at Sleep station, Sleepful or Sleepio
Non-hormonal prescribable medications
Health professionals can prescribe medications which are not hormonal to help relieve hot flushes and night sweats. We need to ensure these medications are right for you, that they will not interact with medication you are taking and that you are aware of any side effects which you might experience and how long the side effects might last.
- Women’s Health concern fact sheet Complementary and alternative therapies
- British Menopause Society: Prescribable alternatives to HRT
Neurokinin 3 receptor antagonists are available privately at the moment and are effective in the relief of hot flushes. This link takes you to the BMS statement.
Supplements over the counter
Please discuss the use of any supplements with your health care professional to ensure they are safe for you to use. If you choose to use herbal medicine, in our opinion at Rowena Health, it is safest to see a medical herbalist. Please refer to the National Institute of Medical Herbalists.
Vitamin D
Vitamin D taken as a 1000 IU daily supplement or obtained from foods such as oily fish and eggs can help reduce joint inflammation, strengthen bones and support cartilage production.
Vitamin D is a fat soluble pro-hormone. It is obtained through the action of sunlight on skin and from the diet. The action of sunlight (ultraviolet radiation wavelength 290–310 nm) on skin converts 7‑dehydrocholesterol to previtamin D3, which is then metabolised to vitamin D3. Dietary vitamin D exists as either ergocalciferol (vitamin D2) or cholecalciferol (vitamin D3).
The liver enzymes convert vitamin D2 and D3 (obtained either from diet or from the action of sunlight on skin) to the main circulating form of the vitamin, 25 hydroxyvitamin D (also known as 25(OH)D). This is then converted by the kidney and other tissues to the active form of the vitamin 1,25-dihydroxyvitamin D.
Magnesium
Extensive food processing reduces the magnesium content of many foods. Good dietary sources include dark chocolate, beans, lentils, nuts, seeds, leafy greens, and whole grains. A systematic review of small observational studies found that magnesium glycinate supplementation (around 350 mg per day) was associated with better sleep quality, including improvements in fatigue, snoring, and sleep duration. Although evidence remains limited, magnesium threonate may also help reduce feelings of anxiety.
Melatonin
Perimenopausal and postmenopausal women have reported improved ability to fall asleep with 2 mg of melatonin. It may also support mood and reduce symptoms of depression although caution is advised in those with autoimmune conditions.
Sage
In a study of 71 women, taking a once-daily tablet containing fresh sage leaves for eight weeks led to a steady weekly reduction in hot flush intensity by about 50% after four weeks and 64% after eight weeks. Sage has proconvulsant effects and should be avoided in people with epilepsy. It may also have mild oestrogen-like properties, so further evidence is needed before recommending it for women with oestrogen-sensitive cancers.
Complementary treatments
It is important to see a qualified specialist in their field if you are considering any therapy.
Mindfulness
Mindfulness-based practices can improve quality of life and are associated with improved sleep quality and perceived stress.
Hypnotherapy
A type of psychological therapy using hypnosis help treat some mental and physical health conditions and to change habits. Reduces vasomotor symptoms and self hypnosis can improve sleep.
Acupuncture:
There is conflicting evidence for benefit but some women report finding this helpful. There may be more benefit for reduction of hot flushes with this treatment in those who have had breast cancer, if treatment is given by a menopause trained practitioner. Evidence also showed an improvement in joint pain in those on aromatase inhibitors.
The British Medical Acupuncture Society
Yoga:
Yoga may have a broad impact on coping with menopausal changes and improving well-being rather than specifically controlling hot flushes.
Herbal medicine
We always recommend you see a specialist to ensure you are taking products that are safe for you.
Treatments they provide can include liquid extracts and tinctures, requiring small, individualised doses.
Examples of herbs they may consider include sage, black cohosh and wild yam for night sweats; chaste tree berry for PMS symptoms; shatavari for hot flushes and vaginal dryness; blue skull cap for anxiety, valerian and passionflower for insomnia, St John’s wort and rose for anxiety, rage and mood swings.
Example of adaptogens (help the body adapt to stress) they may consider include ashwagandha to calm and promote healthy sleep and rhodiola, to improve energy, mood and cognitive function.
Some herbs may interact with medications and need to be taken with guidance if you have medical conditions such as high blood pressure, diabetes, a thyroid condition or a history of hormone sensitive cancer, for example.
Black cohosh may relieve vasomotor symptoms associated with menopause but it can interact with medications, multiple preparations are available, and safety is uncertain
St John’s Wort can relieve anxiety and low mood associated with menopause, but there is uncertainty about variation in nature and potency of preparations. It can interact with other drugs such as anticonvulsants, anticoagulants and tamoxifen. St John’s Wort interacts with HRT and should not be used alongside HRT for this reason.
Download a free guide to herbal medicine

Other sources of information
- The British complementary medicine association
- British Menopause Society short video: Complementary and alternative therapies
- International menopause society – non hormonal treatments
- European Menopause and Andropause Society article
This information is for general guidance and for you to discuss with us at your appointment or your Dr to see if these might be suitable for you. Please do not start to take any of these medications until you have checked they are suitable for you.
Updated November 2025 Dr Carys Sonnenberg
References:


